In a previous article, I wrote about three psychiatric uses cases that can be utilized now for AI applications. One of those use cases, on AI and Patient Similarity, I will now expand upon and write more about it in this article.
As you recall from the previous article on Patient Similarity, a doctor usually utilizes case-based reasoning when encountering a patient. In other words, when a doctor meets with a patient, that doctor immediately compares this patient to other patients the doctor has treated in the past. That way, the doctor is able to determine which treatment is the most appropriate, given how other similar patients were treated from past appointments with the doctor.
Imagine using this case based reasoning to an entire patient database, then utilize computer algorithms to come up with a list of patients who look like the patient in the clinic, the the doctor decides which patients on the list are the most applicable to the patient who now sees the doctor. This process of finding matching patients in the database is called Patient Similarity.
How to Use Patient Similarity in Clinical Practice
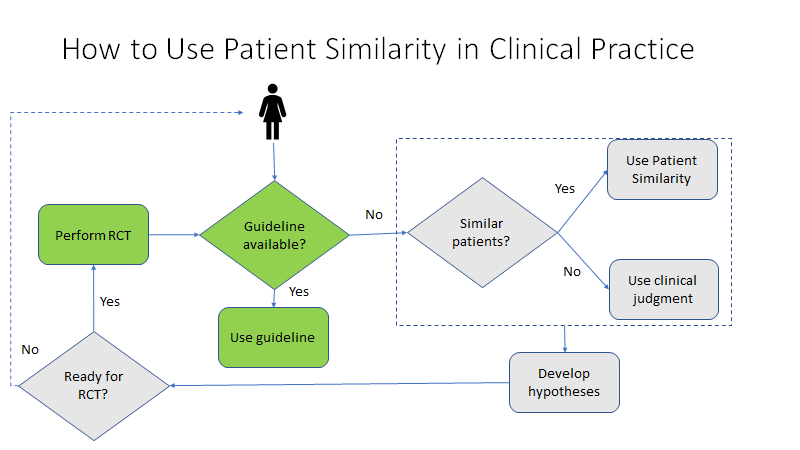
Figure 1 is a flowchart of how Patient Similarity can be used in clinical practice. To begin, suppose you are the doctor and the patient shows up to your clinic. After a medical assessment, the doctor then determines the diagnosis (let’s say Major Depressive Disorder-MDD) and other risk factors associated with the illness (let’s say this patient has maternal uncles who all suicided in their early teens and all have a genetic disorder X), then looks at the above flowchart to determine if clinical guidelines exist for this patient’s condition. If clinical guidelines exist for that disorder, then the doctor follows that clinical guideline to treat the patient.
However, if the patient’s condition does not have a clinical guideline to help inform treatment, then the doctor may consider using AI and do a Patient Similarity search with a computer algorithm, to give a list of potential patients who match the patient’s condition.
So for this patient with [MDD-maternal uncles suicided-genetic disorder X], you find that there is only one matching patient using the Patient Similarity computer algorithm in the patient database you are using. Since there is only one matching patient and not enough other patients to compare treatments, then the doctor is left to use their own clinical judgment to treat the patient’s condition, [MDD-maternal uncles suicided-genetic disorder X]. And if case reports in the literature and other Patient Similarity computer algorithm searches continue to describe new cases of [MDD-maternal uncles suicided-genetic disorder X], the researchers might then opine that this may indeed be a subtype of MDD, or an entirely different disorder. So if they opine this is a subtype of MDD, they might rename this disorder MDD, X subtype.
Sadly, treating patients based on clinical judgment alone is not ideal when treating a potentially life threatening or life altering illness, such as the newly discovered MDD, X subtype. And because MDD, X subtype is newly described, there are no existing clinical guidelines on how to go about with both diagnosis and treatment.
Clearly, it is important to come up with clinical guidelines for this newly described disorder. To remedy this, the doctor may choose to develop a hypothesis regarding why the patient developed this previously unclassified illness, then eventually treat the patient medically, based on the hypothesis and based on how other doctors have been treating this same disorder (using Patient Similarity computer algorithm to find this disorder on other patient databases). Let’s say that addressing the genetic disorder X with medication to alter the abnormal neurotransmitters produced will alter the course of the MDD to make it more amenable to standard MDD treatment.
Then once the hypothesis and treatment are determined for a particular illness (MDD, X subtype), then the doctor can proceed with an RCT (randomized controlled trial) to determine the efficacy and safety of the proposed new treatment. After a few positive RCTs, then this new treatment for this new disorder (MDD, X subtype) can be documented in a clinical guideline, thereby taking the guesswork out of it, and other doctors can follow this new guideline on a previously unstudied illness.
So this is how Patient Similarity utilizing computer algorithms can be used to improve clinical diagnosis and treatment for previously unknown disorders.
Stay tuned for more articles on the AI and Big Data in Psychiatry Series, brought to you by Dr. Carlo Carandang, focusing on the intersection of psychiatry and data science.